The outer Crown of a tooth consists of three layers: enamel, dentin, and pulp. Tooth decay confined to the outer layers is typically resolved with fillings or restorations. However, when decay penetrates the pulp, leading to inflammation or infection, Root Canal Treatment (RCT) or Endodontic Treatment becomes necessary to save the tooth. RCT focuses on removing infected pulp, cleaning, disinfection, filling, and sealing with inert material, followed by restoration and crown placement. This conservative procedure aims to eliminate bacteria, prevent reinfection, and preserve the natural tooth.
Why does one need RCT?
Root canal treatment becomes necessary when bacterial infection damages the tooth pulp beyond the scope of fillings. It addresses infections from sources like cracks, decay, or gum disease. This crucial procedure halts infection spread, saving the tooth from extraction while relieving inflammation-induced pain.
- Intense Tooth Pain: Profound or persistent tooth pain, particularly when chewing or exerting pressure, could indicate the necessity for root canal treatment (RCT).
- Discolouration Darkened or discoloured tooth appearance may signal potential damage or death of the inner pulp.
- Temperature Sensitivity: Heightened sensitivity to hot or cold temperatures, lingering even after the stimulus is removed, might suggest compromised or infected pulp.
- Swelling or Abscess: The swelling or a localised bump on gum tissue adjacent to the affected tooth could indicate an abscess, demanding prompt attention.
- Cracks or Breaks: A cracked or broken tooth is vulnerable to infection, possibly impacting the pulp and warranting RCT assessment
What happens if you don't get an RCT?
Pain Subsiding Doesn't Indicate Healing
Pain relief doesn't signify tooth healing; it suggests dead nerves within the tooth and escalated infection.
Structural Integrity Compromised
Delaying root canal treatment can weaken the tooth's structural integrity, leading to fractures or even tooth loss.
Infection Progression
An untreated infection can spread beyond the affected tooth, potentially affecting neighbouring teeth and causing further dental complications.
Systemic Health Risks
Bacteria from the untreated infection can enter the bloodstream, increasing the risk of systemic health issues such as diabetes, cardiovascular problems, and respiratory infections.
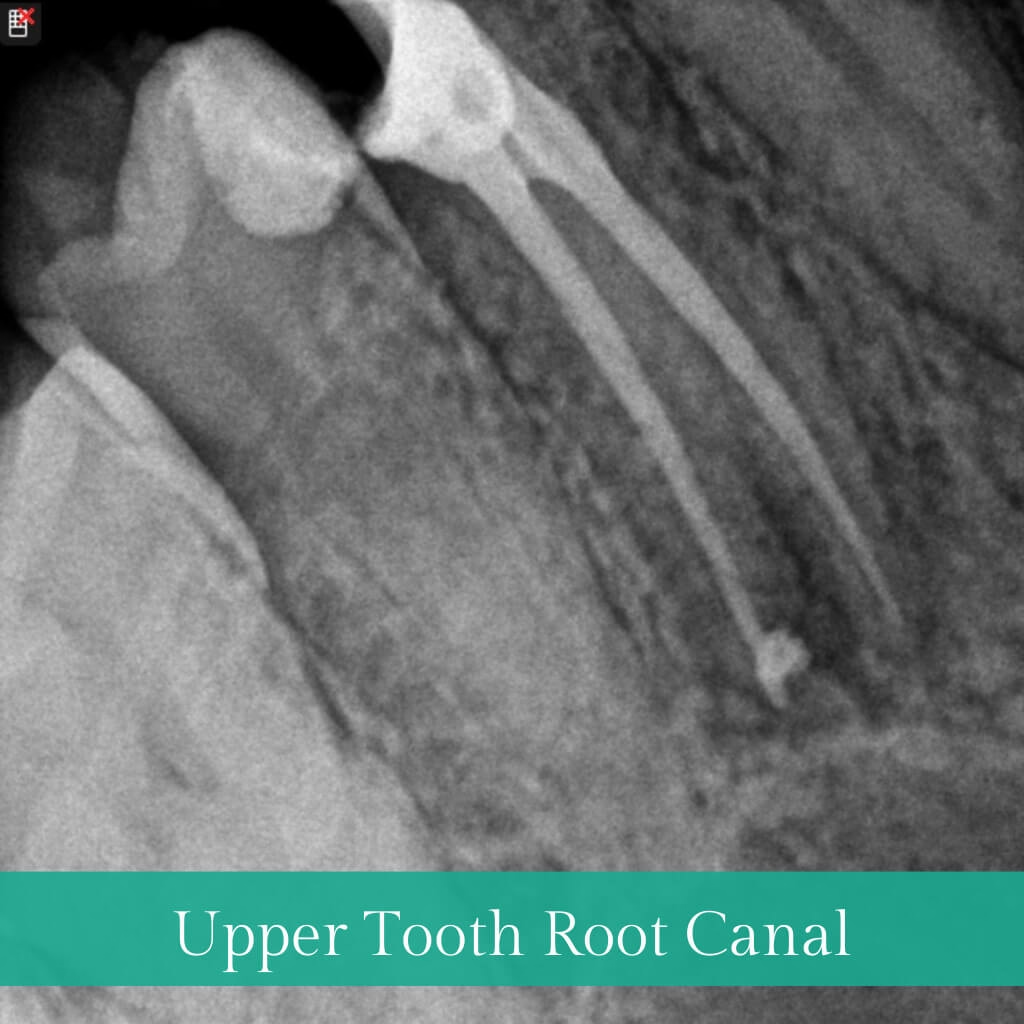
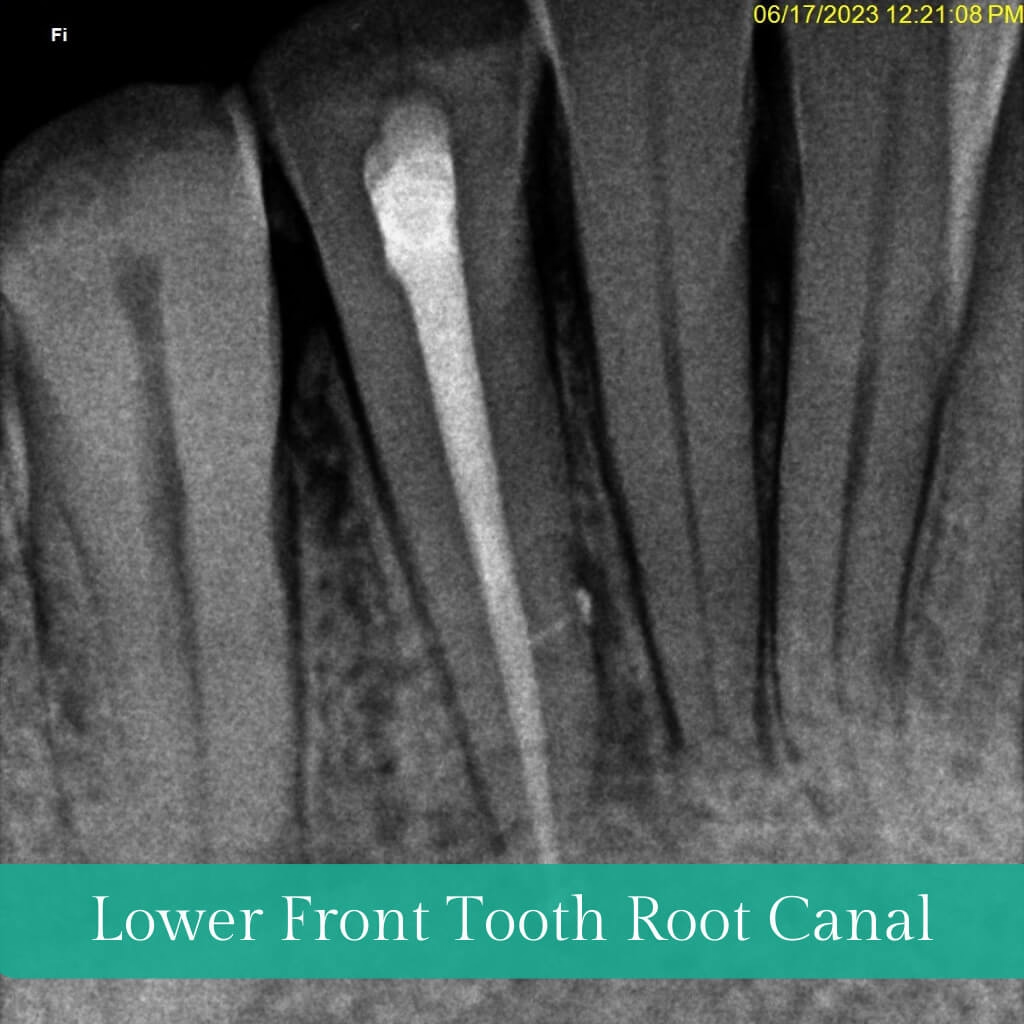
What is the procedure for RCT?
- Initiated with an X-ray for assessment, localised anaesthesia is administered if needed.
- Precise cavity prep clears infected material, ensuring proper pulp access.
- Meticulous disinfection and shaping for thorough cleansing.
- Canals sealed with inert Gutta-Percha to prevent reinfection.
- Depending on the decay, a post and core or Crown may be needed after restoration to conclude the process.
| Myth | Fact |
|---|---|
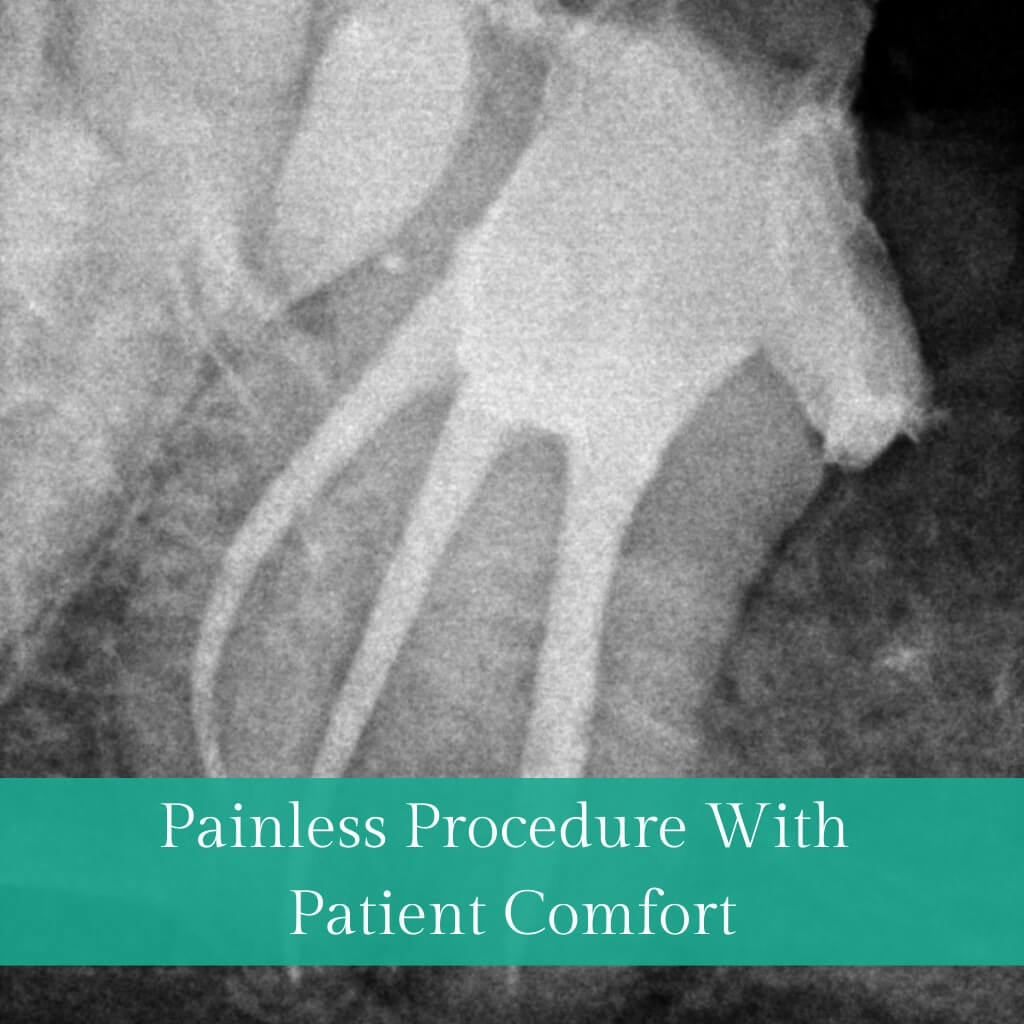
| RCT is painful. | NO! Once the anaesthetic solution is injected, you will not feel any pain or discomfort while the doctor treats your tooth. |
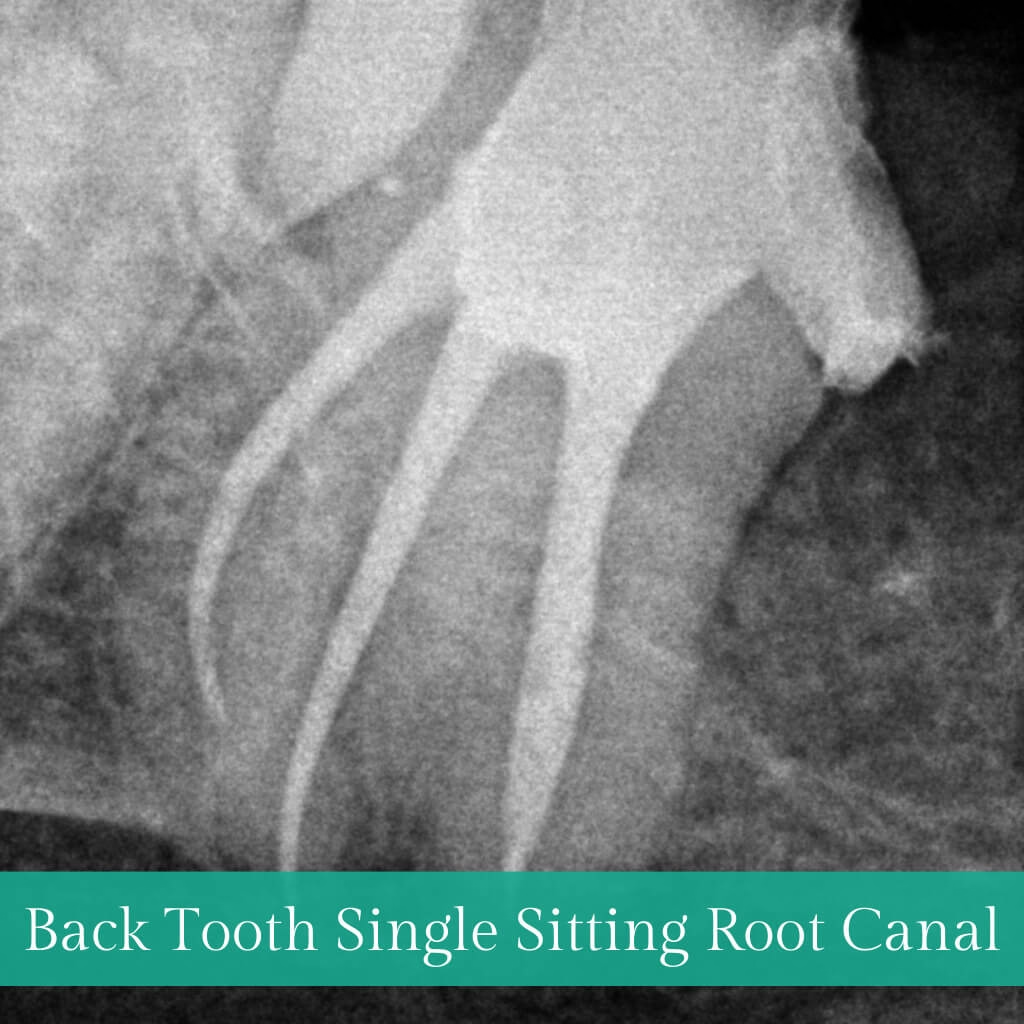
| RCT needs many sittings. | NOT ALWAYS! With advanced technology like rotary instruments and laser-assisted disinfection, RCT can be completed in a single visit lasting 30-60 minutes. |
| RCT makes teeth weak, and they break/ fracture. | NO. Teeth become weak due to decay, which is cleaned during the RCT procedure. When significant decay and loss of natural tooth structure occur, our recommendation to patients is to opt for a crown or cap. This serves as a protective measure, safeguarding the tooth against external forces and the risk of fractures. |
| Removing the tooth is better than RCT. | NO WAY! As doctors, we always strive to preserve and save as much normal and natural structure as we can. Removal of the tooth is the last resort only if the decay or infection is beyond the scope of treatment. |